A Transient Ischemic Attack (TIA), often called a “mini-stroke”, is a temporary period of symptoms similar to those of a stroke. It occurs when there is a brief interruption in blood flow to part of the brain, spinal cord, or retina — typically lasting only a few minutes and not causing permanent damage.
Causes
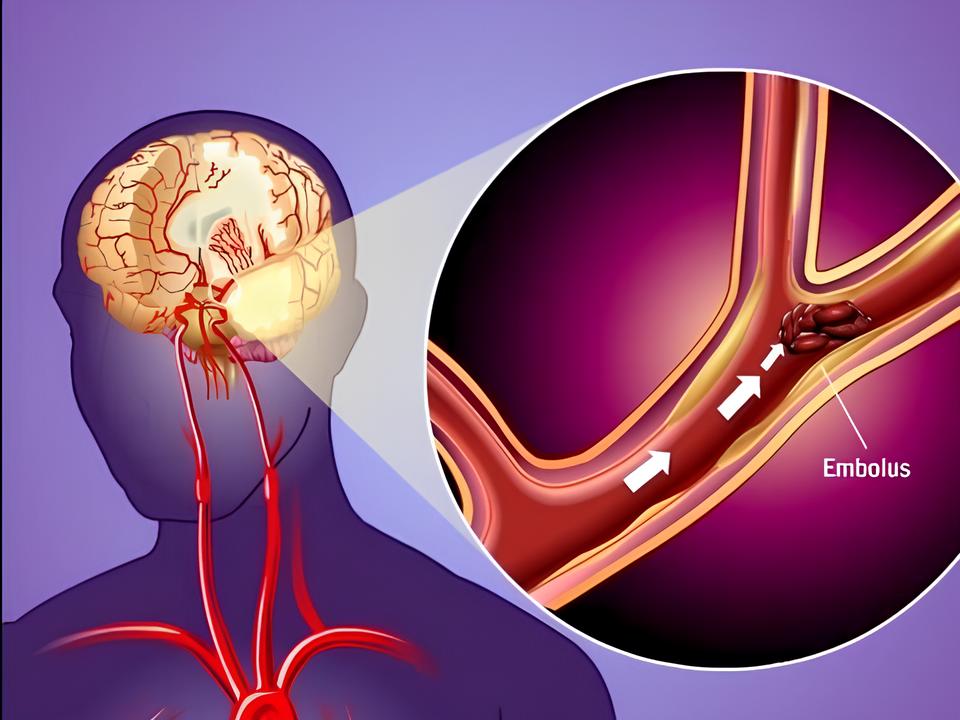
A TIA is caused by a temporary reduction or blockage of blood flow to the brain, usually due to a clot or debris in a blood vessel. Below are the most common causes and contributing factors:
1. Blood Clots (Thromboembolism)
- Embolism from the heart: Common in people with atrial fibrillation or after a heart attack.
- Thrombosis in cerebral arteries: A blood clot forms in a brain artery, often due to atherosclerosis (narrowing from plaque buildup).
2. Atherosclerosis
- Fatty deposits build up in the arteries (especially carotid arteries), narrowing them and increasing the risk of clot formation.
3. Carotid Artery Disease
- Narrowing or blockage in one or both carotid arteries (major blood vessels in the neck supplying the brain).
4. Cardiac Causes
- Atrial fibrillation (irregular heartbeat)
- Heart valve disease
- Heart failure
- Recent heart surgery
These conditions can produce clots that travel to the brain (cardioembolic TIA).
Clinical features
The clinical features of a TIA refer to the observable signs and patient-reported symptoms that clinicians use for diagnosis. These features are often transient, lasting less than 24 hours, and depend on which part of the brain is affected.
General Clinical Features
- Sudden onset of symptoms
- Short duration (minutes to a few hours)
- Complete resolution of symptoms within 24 hours
- No permanent neurological deficits on examination after resolution
Neurological Features by Affected Area
| Brain Region | Clinical Features |
|---|---|
| Middle cerebral artery (MCA) territory | Hemiparesis (face/arm > leg), hemisensory loss, aphasia (if dominant hemisphere), neglect (if non-dominant) |
| Posterior circulation (vertebrobasilar system) | Dizziness, vertigo, diplopia (double vision), dysarthria, ataxia, bilateral weakness, drop attacks |
| Retinal (amaurosis fugax) | Sudden, painless, transient vision loss in one eye (often described as a “curtain coming down”) |
| Internal carotid artery | Mixed symptoms: monocular blindness, hemiparesis, hemisensory loss, aphasia |
Diagnosis
- Clinical evaluation
- Imaging like MRI or CT scan
- Carotid ultrasound, echocardiogram, and blood tests
Physiotherapy management
Although a TIA causes no lasting neurological damage, physiotherapy management is essential for:
- Early recovery from transient impairments (e.g., balance, weakness)
- Stroke prevention through lifestyle modification and exercise
- Patient education and risk factor management
Assessment Phase
Before initiating treatment:
- Detailed functional assessment:
- Muscle strength, tone, joint mobility
- Balance and gait (Berg Balance Scale, Tinetti)
- Functional mobility (Timed Up and Go)
- Cardiovascular fitness (6-minute walk test)
- Neurological screening:
- Cranial nerves, reflexes, coordination, sensation
- Fall risk evaluation
Goals
| Short-Term Goals | Long-Term Goals |
|---|---|
| Improve balance and mobility | Prevent stroke recurrence |
| Enhance muscle strength | Promote cardiovascular fitness |
| Reduce fear of falling | Improve quality of life and independence |
| Educate on lifestyle changes |
Core Physiotherapy Interventions
A. Balance & Gait Training
- Static balance: Single-leg stance, tandem standing
- Dynamic balance: Heel-to-toe walking, direction changes, obstacle walking
- Gait re-education: Use of walking aids, step length & pattern correction
B. Strengthening Exercises
- Focus on major muscle groups: quadriceps, hamstrings, glutes, core
- Progressive resistance training (e.g., bodyweight, resistance bands, weights)
- Frequency: 2–3 sessions/week, 10–15 reps × 2–3 sets
C. Cardiovascular Training
- Aerobic exercise (e.g., brisk walking, cycling, treadmill)
- Intensity: Moderate (50–70% of max HR), monitored closely
- Duration: Start with 15–20 minutes, build up to 30–40 minutes, 3–5x/week
D. Flexibility and Postural Control
- Stretch tight muscle groups (e.g., calves, hamstrings, hip flexors)
- Postural exercises to correct alignment and reduce fatigue
E. Proprioception and Coordination
- Balance boards, foam pads
- Hand-eye and lower limb coordination drills
F. Functional Mobility Training
- Bed mobility, sit-to-stand, chair transfers
- Practicing real-world tasks to promote confidence
4. Patient Education
Medication adherence (e.g., antiplatelets)
Stroke warning signs (Be fast)
Importance of medical follow-up (e.g., for atrial fibrillation, hypertension)
Home exercise program and self-monitoring
Risk factor management:
Smoking cessation
Weight loss and diet
Stress management
Medication adherence (e.g., antiplatelets)