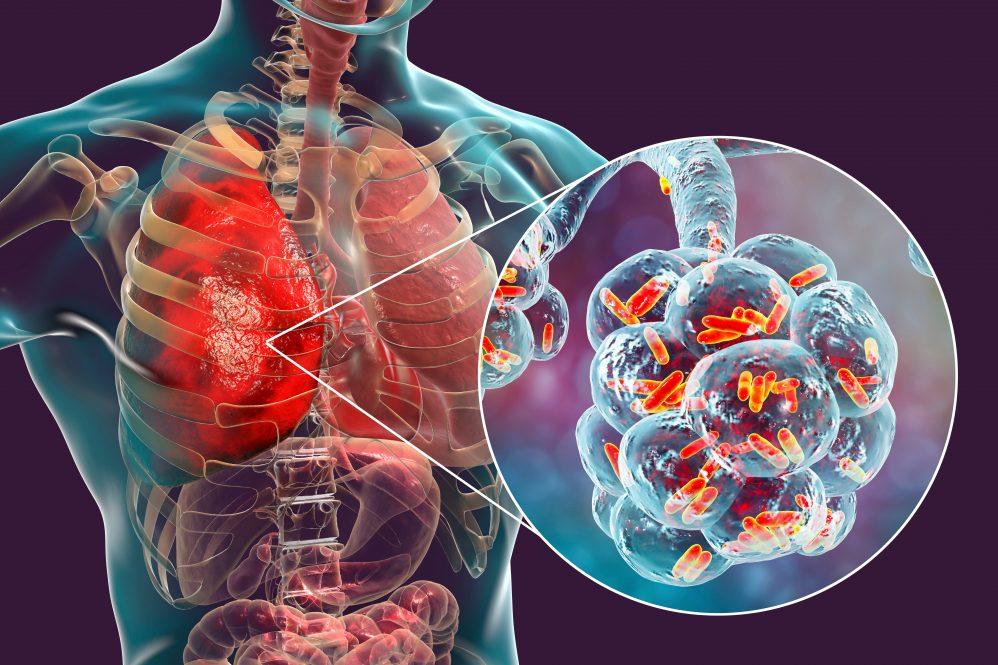
Pneumonia is an infection that causes inflammation and fluid buildup in the lungs. It can be triggered by bacteria, viruses, fungi, or, in rare cases, protozoa. This condition can make breathing difficult and lead to symptoms such as fever, cough, and mucus production.
Causes of pneumonia
Pneumonia is classified based on its cause and where it was acquired:
- Bacterial Pneumonia: Often more severe than viral pneumonia, commonly caused by Streptococcus pneumoniae.
- Viral Pneumonia: Usually less severe, caused by viruses like influenza, RSV, or COVID-19.
- Fungal Pneumonia: Affects individuals with weakened immune systems.
- Aspiration Pneumonia: Results from inhaling food, liquid, or vomit into the lungs.
Pneumonia can also be categorized based on where it was contracted:
- Community-Acquired Pneumonia (CAP): Contracted outside of healthcare settings.
- Hospital-Acquired Pneumonia (HAP): Acquired during a hospital stay, often caused by antibiotic-resistant bacteria.
- Ventilator-Associated Pneumonia (VAP): Occurs in patients on mechanical ventilation.
Symptoms of pneumonia
Pneumonia symptoms vary depending on the cause and the patient’s age. Common symptoms include:
- Fever, chills, and sweating
- Persistent cough with yellow, green, or bloody mucus
- Shortness of breath or rapid breathing
- Chest pain that worsens with coughing or deep breathing
- Fatigue and weakness
- Cyanosis (bluish skin, lips, or nails)
- Confusion (especially in older adults)
- Headache and muscle aches
- Loss of appetite
- Nausea, vomiting, or diarrhea (more common in children)
Diagnosis of Peumonia
To diagnose pneumonia, healthcare providers perform:
- Physical Exam: Listening to lung sounds with a stethoscope to detect abnormal breathing patterns such as crackling or wheezing.
- Chest X-ray or CT Scan: To detect lung inflammation, consolidation, or fluid accumulation.
- Blood Tests: To identify infections, check for elevated white blood cell counts, and detect pathogens in the bloodstream.
- Sputum Test: To analyze mucus from the lungs and determine the specific pathogen causing the infection.
- Pulse Oximetry: To measure blood oxygen levels and assess respiratory efficiency.
- Bronchoscopy (in severe cases): A procedure using a thin, flexible tube with a camera to examine the airways and collect lung samples.
- Arterial Blood Gas (ABG) Test: Measures oxygen and carbon dioxide levels in the blood to evaluate lung function.
Physiotherapy management
Physiotherapy can play an essential role in managing pneumonia, especially in improving lung function, clearing mucus, and preventing complications like lung collapse (atelectasis).
Goals
- Improve lung ventilation (breathing capacity)
- Assist in mucus clearance (reduce congestion)
- Enhance oxygenation
- Prevent complications (like lung infections, atelectasis)
- Strengthen respiratory muscles
Physiotherapy Techniques for Pneumonia
1. Breathing Exercises
These help improve lung expansion and oxygen intake:
- Diaphragmatic Breathing (Belly breathing) – Encourages deep breathing and improves oxygen exchange.
- Pursed-Lip Breathing – Helps control shortness of breath and improve oxygenation.
- Incentive Spirometry – A device to encourage deep breathing and prevent lung collapse.
2. Airway Clearance Techniques
- Postural Drainage – Positioning the patient to drain mucus from the lungs.
- Percussion (Clapping) – Gentle tapping on the chest to loosen mucus.
- Vibration Techniques – Helps move mucus upward for easier coughing.
- Active Cycle of Breathing Technique (ACBT) – A combination of breathing control, deep breaths, and huffing to clear mucus.
3. Coughing Techniques
- Huff Coughing – Controlled coughing to remove mucus without straining the lungs.
- Assisted Coughing – A therapist or caregiver helps with forceful coughing.
4. Mobility & Exercise Therapy
- Early Mobilization – Encourages movement to prevent complications.
- Walking & Light Exercises – Helps improve lung capacity and overall recovery.
- Gradual Strength Training – Strengthens respiratory muscles and overall endurance.
5. Oxygen Therapy & Chest Expansion Exercises
- Used for severe cases to improve breathing efficiency.
Precautions During Physiotherapy
- Avoid aggressive techniques in fragile patients.
- Monitor oxygen levels and breathing difficulty.
- Stop if the patient experiences dizziness, pain, or extreme breathlessness.